It is universally and scientifically accepted that prostate cancer occurs in asymptomatic men or as an incidental finding later in life. Prostate cancer is the second leading cause of male cancer deaths. About 250,000 cases occur in the USA alone. Until now we have used the digital rectal screening exam and the serum PSA (prostate-specific antigen). Discrepancies as to how to use these tools have occurred domestically and internationally. This makes the decision regarding definitive treatments (e.g. nothing, surgery, radiation, hormone therapy, chemotherapy) all challenging.
Distinguishing which cancers are aggressive, and which are nonaggressive, has relied previously on sonographic guided biopsy using Trans Rectal Ultrasonography (TRUS). The Gleason score has been used pathologically after biopsy to determine which cancers have aggressive potential (Gleason 6 or greater, more aggressive).
Preparation for the Exam
Protocol at 1.5 Tesla for Prostate
(see below but add 3D if mapping with TRUS for biopsy is under consideration)
Imaging Introduction
A five-point scoring system has been developed based on a combination of mpMRI (multi-parametric MRI) findings that consist of:
Pearls Regarding Technique
Sample Cardiac Coil Non-endorectal Prostate Study

T1WI: TSE T1w TSE; FOV = 420mm; 512 matrix; 1.0 x 1.2 mm pixel size; 38 slices of 3.5 mm; SENSE FACTOR 2; TR = 600; TE = 8; TF = 4; Scantime 1:21

Coronal T2WI TSE/FSE: TSE T2w TSE; FOV = 200 mm; 512 matrix; 0.5 x 0.7 mm pixel size; 24 slices of 3.5 mm;TR = 3200; TE =130; TF = 24; Scantime 3:48

Axial T2WI FSE/TSE: 2 slices shown: FOV = 200 mm; 512 matrix; 0.6 x 0.7 mm pixel size; 24 slices of 3.5 mm; TR = 3200; TE = 130; TF = 24; Scantime 4:26

Dynamic Contrast-enhanced MRI DCE MRI: Images acquired from the first 6 dynamic 3D acquisitions; 3D T1 TFE with SPIR; FOV = 420 mm; 256 matrix; 1.6 x 1.6 mm pixel size; 30 slices of 3.5 mm; SENSE FACTOR 2;TR = 4.8;TE = 2.4; FA = 10; Scantime 13.5s/3D


Diffusion Imaging should be performed on all prostate cancer patients undergoing MRI using multiple b-values. The highest b-value should exceed 1,200-1,400. Cancers diffusion restrict, therefore, they get brighter as the b-value is increased (and darker on the ADC map). Generalized causes of diffusion restriction include:
Thus, the causes of false positive or negative diffusion MRI in prostate cancer include:
Opinion Position Statement Regarding Field Strength and Endorectal Coil Imaging
“In the past, 3.0 Tesla MR system was recommended for examination of prostate cancer because of higher SNR, spectroscopy and it enables high quality imaging within a short time without the use of an endorectal coil.
This is no longer supported by data or practitioners who are active in the field with proper prep and newer technology. Spectroscopy has, for now, become a research tool, coil technology is superior at 1.5 T, artifacts are fewer, isotropic 3D mapping TSE/ FSE is excellent at 1.5 T. Finally, technology has evolved such that endorectal coil imaging is no longer needed for a quality exam and is not viewed favorably by patients.”
Screening Options for Prostate MRI: Position Statement for Consideration
Axial 2D T2 FSE + Diffusion + DCE MRI is a 20 minute screening exam and very economical for the patient.
Advantages:
This has been referred to as “Abbreviated Biparametric Prostate MR”
Kuhl CK. Et al. Radiology 285(2) p. 483
In this long term study by a respected expert in Germany on DCE MRI the detection rate for “clinically significant” prostate lesions was equal to “full” parametric MRI.
In her study of over 500 patients, gadolinium enhanced DCE MRI is also eliminated. DCE MRI is only used as a major criterion to “characterize lesion” in PZ (peripheral zone lesions), and this eliminates the need for IV access and saves time. Total scan time is under 10 minutes. Additionally in this study, ALL PI-RAD 3s were biopsied (which would normally not be the case). 93.5% were benign.
Disadvantages: If an aggressive lesion is found, the patient must return for diagnostic 3 planar MRI with 2D or 3D technique for purposes of TRUS / MRI guided biopsy. T staging with the abbreviated study is less accurate. Localization in the gland requires more expertise. Still, detection of aggressive significant cancers is equal between the two techniques.
The main function of the prostate is to secrete prostatic fluid. Prostatic fluid is a key component of semen, and during ejaculation, prostate muscles contribute to propulsion of the semen through the urethra.
From the base of the bladder to the membranous urethra, the prostate envelopes the prostatic urethra. Within the lesser pelvis, the prostate is located behind the inferior border of the symphysis pubis and pubic arch, and anterior to the rectal ampulla.
Prostate is divided into three major compartments:

Coronal and axial, planar
 Sono with Doppler, hypervascularity favors tumor- 85% of aggressive tumors Gleason 8, 9, 10 have hypervascularity
Sono with Doppler, hypervascularity favors tumor- 85% of aggressive tumors Gleason 8, 9, 10 have hypervascularity
Coronal surface rendered front view

Coronal anatomic Descriptors:
Base = Proximal; Distal = Apical
Mid is divided into intermediate or int. (closer to the midline) and lat. or more lateral

Sagittal
Note: All ages are approximate
Birth
Birth to 12-14 years
12-14 to 17-18 years
17-18 years to 30 years
30 to 39 years
40 to 44 years
45 to 50 years
After 50 years
Click here to see a case example of PI-RADS 1
Click here to see a case example of PI-RADS 2
Click here to see a case example of PI-RADS 3
Click here to see a case example of PI-RADS 4
PI-RADS utilizes a 5-point scale based on the probability that a combination of mpMRI findings on T2W, DWI, and Dynamic Contrast Enhanced (DCE) images correlate with clinically significant prostate cancer.




PI-RADS v2 has flaws, i.e. a TZ lesion can be moved from a 2 to 4 category with slight changes in T2 morphology. The following are links to some publications about this:
https://pubs.rsna.org/doi/pdf/10.1148/rg.313105139
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4656245/pdf/13244_2015_Article_426.pdf
https://link.springer.com/content/pdf/10.1007%2Fs13244-017-0578-x.pdf
PROMIS study: For clinically significant cancer, MP-MRI was more sensitive (93%) than TRUS-biopsy (48%). 37% negative TRUS still had clinically significant Ca. MR can avoid biopsy in 27% of men with high PSA.
Anatomy PEARL: Central zone tumours are rare, hard to detect as CZ normally is hypo on T2 and restrict. Symmetry is key (18% CZ is asymmetrical), Also CZ does not extend below veromontanum!
How to do it: Mention up to 4 most suspicious lesions in report, and include index lesion. Index lesion is Highest PI-RADS >> EPE (Extraprostatic extension) >> Size. Lesion size is largest axial dimension measurement.
PIRAD PERSONAL PEARL: PSA density of > 0.2 ng/ml is suspicious, should consider biopsy irrespective of MR results, unless there has been prostatitis or instrumentation. Conversely, PSA density <0.1 ng/ml is usually benign.
Therefore if you are contemplating PI-RADS 3 (2 or 4) and PSA density is > 0.2ng/ml err on the side of PI-RADS 4. If PSA density is < 0.1 ng/ml err towards PI-RADS 2 and follow-up in one year.
PI-RADS 3 Pearl: A PI-RADS 3 upgraded to 4 using either DCE or ADC correlated with better clinical outcome than an initial PI-RADS 4, ie PI-RADS 3+1 is not equal to a 4
|
Score |
Peripheral Zone (PZ) |
|
1 |
Uniform hyperintense signal intensity (normal) |
|
2 |
Linear or wedge-shaped hypointensity or diffuse mild hypointensity, usually indistinct margin |
|
3 |
Heterogeneous signal intensity or non-circumscribed, rounded, moderate hypointensity Includes others that do not qualify as 2,4, or 5 |
|
4 |
Circumscribed, homogeneous moderate hypointense focus/mass confined to prostate and <1.5cm in greatest dimension |
|
5 |
Same as 4 but ≥ 1.5cm in greatest dimension or definite extra prostatic extension/invasive behavior |
|
PEARL |
Extruded BPH nodules can mimic PZ lesions, known pitfall. |
|
Score |
Transition Zone (TZ) |
|
1 |
Homogeneous intermediate signal intensity (normal) |
|
2 |
Circumscribed hypointense or heterogeneous encapsulated nodule(s) (BPH) |
|
3 |
Heterogeneous signal intensity with obscured margins Includes others that do not qualify as 2,4, or 5 |
|
4 |
Lenticular or non-circumscribed, homogeneous, moderately hypointense, and <1.5 cm in greatest dimension |
|
5 |
Same as 4, but ≥1.5cm in greatest dimension or definite extraprostatic extension/invasive behavior |
|
Score |
Peripheral Zone (PZ) or Transition Zone (TZ) |
|
1 |
No abnormality (i.e., normal) on ADC and high b‑value DWI |
|
2 |
Indistinct hypointense on ADC |
|
3 |
Focal mildly/moderately hypointense on ADC and isointense/mildly hyperintense on high b-value DWI |
|
4 |
Focal markedly hypointense on ADC and markedly hyperintense on high b-value DWI; <1.5cm in greatest dimension |
|
5 |
Same as 4 but ≥1.5cm in greatest dimension or definite extraprostatic extension/invasive behavior. |
|
PEARL |
T2 Blackout effect: lesions with very short T2 or T2* values create blackout phenomenon on T2, ADC and DWI. Tumors are not black, they are gray. T2 blackout can be due to paramagnetic effect. |
|
PEARL |
PZ in younger pt normally shows mild symmetrical restricted diffusion due to higher glandular density.
|
Principle of Computed DWI – (Diffusion – weighted imaging)
The computed DW imaging (cDWI) is a mathematical method in which b-value is calculated from two real DW images with different b-values.
The apparent diffusion coefficient (ADC) is calculated with the following equation:
ADC=In[-S/So]/(b-bo)
Using two real DWI signals in a monoexponential model, signals on arbitrarily set b-value are calculated with the following equation:
Sc=Soexp[-(bc-bo)ADC]
|
Score |
Peripheral Zone (PZ) or Transition Zone (TZ) |
|
(-) |
No early enhancement, or diffuse enhancement not corresponding to a focal finding on T2 and / or DWI or focal enhancement corresponding to a lesion demonstrating features of BPH on T2WI |
|
(+) |
Focal, and; earlier than or contemporaneously with enhancement of adjacent normal prostatic tissues, and; corresponds to suspicious finding on T2W and / or DWI |
|
PEARL |
Prostatitis and BPH can show early enhancement and washout |
|
DWI |
T2W |
DCE |
PI-RADS |
|
1 |
Any |
Any |
1 |
|
2 |
Any |
Any |
2 |
|
3 |
Any |
(-) (+) |
3 4 |
|
4 |
Any |
Any |
4 |
|
5 |
Any |
Any |
5 |
|
DWI |
T2W |
DCE |
PI-RADS |
|
1 |
Any |
Any |
1 |
|
2 |
Any |
Any |
2 |
|
3 |
≤4 5 |
Any Any |
3 4 |
|
4 |
Any |
Any |
4 |
|
5 |
Any |
Any |
5 |
PEARL 1: TZ cancers almost never develop posteriorly, usually anterior half and in the apical third. Caveat is the tumor in the anterior half is so big it extends into the posterior half
PEARL 2: . A good sign of benign TZ nodules are microcysts (discreet foci of T2 hyperintensity), this is correlated by pathologic histology and are dilated hyperplastic acini.
PEARL 3: Negative predictive value for MR prostate done well and read well is 90% for Gleason 3+4 and above, and more than 90% for 4+3 and above.
PEARL 4: AS & CZ zone lesions are a gray “difficult” area (sorry for the pun!). It is not clear which parameter to use but use ADC first and then early b value DCE to assess further
PEARL 5: TZ tumors tend to be lower grade, don't overcall TZ lesions. Look for excuse not to call a tumor in the TZ.
PEARL 6: DCE is useful in 10% of cases as a second line of defense in case of initially missed DWI or T2 lesion, Especially if DWI faisl from metal or post-focal radiation or other pitfalls like air in the rectum.
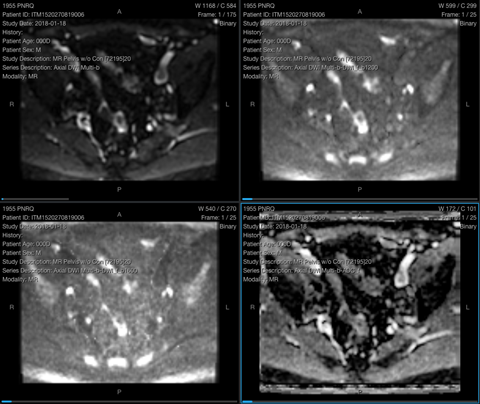
This 62-year-old male presents with prostate-specific antigen (PSA) of 6.44.


Image 1 - Axial T2 FSE / TSE 2D Image 2 - Diffusion MRI b1500
(3mm)


Image 3 - Parametric ADC Map Image 4 - DCE MRI Phase 5
(60 seconds post-injection)
The prostate is 4.7cm in transverse dimension, 3.9cm in AP dimension, and 4.8cm in craniocaudal dimension. No areas of restricted diffusion or hypointensities in the peripheral zone. Generalized ill-defined non mass-like moderate hypointensity in the transitional zone. Small cystic nodule at the anterior right transitional zone. The capsule intact. Seminal vesicles and neurovascular bundles normal in appearance.
No lymphadenopathy in the pelvis. No focal abnormal signal intensity in the osseous structures. A 1.3 x 1.5 x 1cm fluid intensity abutting the anterior inferior left acetabulum probably is a paralabral cyst. Arthrosis of the pubic symphysis.
CONCLUSION:
No focal hypointense mass or areas of restricted diffusion, PI-RADS 1.
Click here to launch this case


Follow this link for a video example of PI-RADS 1: https://mrionline.proscan.com/courses/prostate/lectures/5173451
Make sure to check out the:
Related Case(PI-RADS 1)
This 62-year-old male presents with elevated prostate-specific antigen (PSA) level measuring 8.3ng/mL.


Image 1 - Axial T2 Image 2 - Axial
BPH, TZ hypertrophy (1mm) Parametric ADC map, TZ hypertrophy,
Contiguous, 3D TSE / FSE BPH, no low signal velocity restriction
particularly in PZ


Image 3 - Axial DWI Image 4 - Axial DCE MRI with Gadolinium,
Diffusion, b1600, TZ hypertrophy, 8 seconds after injection, scattered TZ
BPH, No high signal diffusion enhancement of low amplitude(arrows)
restriction in PZ
The prostate gland measures 6cm in CC, 5cm in AP, and 6cm in RL dimensions. Calculated prostate volume is 94cc and PSA density is 0.09. Transitional zone hyperplasia is present. Stromal hyperplasia areas demonstrate mild to moderate diffusion restriction. No suspicious T2 hypointensity with substantive diffusion restriction to suggest malignant neoplastic process in the transitional zone. Peripheral zone demonstrates linear T2 hypointense scarring regions. Anatomical prostate capsule, bilateral neurovascular bundles, rectoprostatic angles and seminal vesicles are clear.
No lymphadenopathy in the pelvis or inguinal regions. Subcentimeter in diameter right external iliac chain lymph node is noted. Mild diverticular disease of the sigmoid colon without evidence of acute diverticulitis. Rectal wall is unremarkable. Visualized musculoskeletal structures are within normal limits. Urinary bladder is partially full and demonstrates mild wall thickening. No pseudo diverticula formation.
CONCLUSION:
Additional diffusion-weighted images through the prostate are obtained. No substantive diffusion-restricted, T2- hypointense region in the transitional or peripheral zone of the prostate gland to suggest malignant neoplastic process.
Click here to launch this case

Follow this link for a video example of PI-RADS 2: https://mrionline.proscan.com/courses/prostate/lectures/5173461
Make sure to check out the:
Related Case(PI-RADS 2)
This 72-year-old male presents with elevated prostate-specific antigen (PSA).


Image 1 - Axial DWI, b1600 (arrows) Image 2 - Axial DWI (arrows)


![]()
Image 3 - Axial T2 FSE / TSE (arrow) Image 4 - Axial TIGRE
2D (3mm) DCE MRI Phase 1 (10 seconds) No hypervascularity in area of diffusion restriction in left mid TZ
The prostate measures 7.6 x 6.0 x 7.1cm for an estimated volume, using the ellipsoid formula, of 169.4cc and tumor density of 0.062 ng/mL/cc which is at the lower end of the indeterminate risk range.
Peripheral Zone: Bilobed diffusion restricting signal abnormality within the right mid gland PZpa measuring 1.7 x 1.0cm with greater than a centimeter of capsular contact but no extracapsular extension. There is vascularity in this region but no corresponding T2 signal abnormality. PI-RADS 3.
Central Gland: Bilobed 10 x 7mm lesion in the central gland TZp mid prostate near the midline and a second area in the lateral aspect of the left midgland TZp on the same key image, this lateral lesion measuring 9 x 5mm. The vascularity is equivocal. No corresponding T2 lesion.
Normal rectoprostatic angles and neurovascular bundles. The left seminal vesicle is desiccated. The right is normal. Normal space of Retzius. Prostatomegaly protruding into the bladder trigone. Bladder wall thickening compatible with outlet obstruction. No lymphadenopathy or bone lesion.
CONCLUSION:
Click here to launch this case


Follow this link for a video example of PI-RADS 3: https://mrionline.proscan.com/courses/prostate/lectures/5173478
This 64-year-old male presents with increasing prostate-specific antigen (PSA) from 5.07 to 9.00 in seven months.


Image 1 - Axial T2 FSE / TSE (arrow) Image 2 - Coronal T2 FSE / TSE (arrow)
(3mm) 2D, nodule left PZ pl (base) (3mm) 2D, nodule left PZ pl (base)


Image 3 - Axial DWI (arrow) Image 4 - Axial DWI (arrow)
Diffusion b-1600, hyperintense ADC parametric map shows low
diffusion restriction left PZpl (base) signal velocity
restriction left PZpl (base)
The prostate measures 3.5 x 3.5 x 4.6cm for an estimated volume, using the bullet formula, of 37cc and tumor density of 0.246ng/mL/cc which is in the high risk range.
Peripheral Zone: Diffusion restricting crescent T2 hypointensity in the left base measuring 1.0 x 0.6cm involving the entrance of the left seminal vesicle. No right-sided lesion in the peripheral zone.
Prostate utricle cyst.
Central Gland: CZ/TZ hypertrophy with bladder wall thickening compatible with outlet obstruction. Innumerable T2 hypointensities and patchy areas of diffusion restriction, too numerous to count, favored to reflect hyperplastic nodules without suspicious lesion.
Heterogeneous vascularity throughout the prostate. No lymphadenopathy or bone lesion. Colonic diverticulosis. Mild symphysis pubis arthrosis. Normal space of Retzius. Normal rectoprostatic angles.
CONCLUSION:
Click here to launch this case


Follow this link for a video example of PI-RADS 4: https://mrionline.proscan.com/courses/prostate/lectures/5182284
Make sure to check out the:
Related Case(PI-RADS 4)
This 63-year-old male presents with elevated prostate-specific antigen (PSA).


(2.5mm) apex to base right hyperintensity right relative to leftImage 1 - Axial 2D T2 FSE / TSE Image 2 - Diffusion b-1600 (arrows)
isointense mass over 2cm gland consistent with diffusion
with extensivecapsular contact restriction more easily seen on
ADC map


Image 3 - ADC b-1600 Image 4 - DYN THRIVE(arrows) parametric map (arrows)
shows low signal right gland DCE MRI post contrast Phase 1
velocity restriction (7 seconds) (4mm) with 50% overlap; pronounced enhancement right gland
The prostate is 4.2cm in transverse dimension, 3.5cm in AP dimension and 3.5cm in craniocaudal dimension. A uniformly hypointense mass throughout the right hemisphere involving both the peripheral zone and central gland from apex through the base with probable areas of crossing midline. There is suggestion of extension to the base of the seminal vesicle. Subtle irregularity of the right side capsule probably represents transcapsular extension. The neurovascular bundle appears spared. Moderate restricted diffusion of the lesion with early and persistent enhancement. A fluid intensity posterior of midline probably is utricle cyst.
No direct invasion through the urinary bladder. No lymphadenopathy in the visualized pelvis. Bilateral small inguinal hernia with fat. Visualized osseous structures normal in signal intensity.
CONCLUSION:
Click here to launch this case


Follow this link for a video example of PI-RADS 5: https://mrionline.proscan.com/courses/prostate/lectures/5182285
Patient must qualify for surveillance by way of the Epstein Inclusion Criteria and Tiers of Assessment (i.e. Gleason, PSA, Tumor count).
The Epstein Inclusion Criteria was developed in 1994 for the purpose of assessing prostate cancer significance.
Insignificant prostate cancer was defined as having a tumor volume less than 0.2cm3, organ-confined, and no Gleason patterns 4 or 5. Being characterized as a ‘minimal tumor’ implied that the tumor volume was 0.2-0.5cm3. Oon
As originally defined by Epstein in the validation studies, the optimum preoperative criteria were:
Example of a study showing Apparent Diffusion Coefficient (ADC) values and their Gleason Score Correlation (more studies are still needed to validate)
|
Gleason Score |
Number of Tumors |
Least-Squares Mean |
Standard Error of Mean |
Range - ADC (x10-3 mm2/s) |
|
6 |
25 |
0.860 |
0.036 |
0.659-1.263 |
|
7 |
37 |
0.702 |
0.030 |
0.108-0.963 |
|
8 |
10 |
0.672 |
0.057 |
0.417-0.875 |
|
9 |
9 |
0.686 |
0.067 |
0.534-0.848 |
Pathology - Malignant Neoplasms
|
Grade 1 |
Tumor composed of well-defined individual glandular nodules, closely arranged, uniform and separate from each other |
|
Grade 2 |
Tumor still relatively well defined, but with possible minimal extension of the neoplastic acini to the periphery of the tumor nodule in the noncancerous prostatic tissue |
|
Grade 3 |
Tumor infiltrates the noncancerous prostatic tissue; the gland shows marked variation in size and organization |
|
Grade 4 |
Markedly atypical cells with extensive infiltration into surrounding tissues |
|
Grade 5 |
Tumor presents no glandular differentiation; composed of sheets of undifferentiated cancer cells |
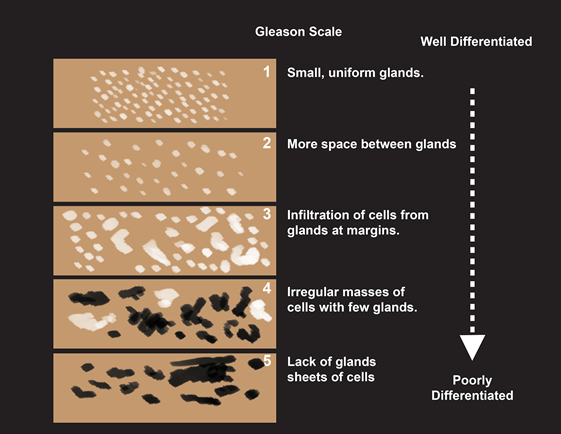
The score is defined by the combination of the primary predominant grade, and the secondary grade. Its range is potentially from 2 (1+1) to 10 (5+5). A score of 2 to 4 in biopsies is rare: these are generally lesions present in the transition zone which are sampled during transurethral resection of the prostate (TURP). The Gleason grade is reported for each individual biopsy sample, and the biopsy with the highest grade is considered representative of the Gleason score of the patient. Patients can have a well-differentiated tumor (Gleason score 2 to 4), moderately differentiated (5 to 7), or poorly differentiated (8 to 10). However, it should be borne in mind that a Gleason score of 4+3=7 is different from 3+4=7, because, although the sum is the same, in reality the first case has a higher primary grade. In other words, the Gleason 4 is in more samples or “chips” than the Gleason 3 in the 4+3=7 scenario. Therefore, this is a more serious scenario than the 3+4=7.
In addition to the primary and the secondary grades, the tumor also shows a tertiary grade which is higher than the other two. Despite being less represented, this tertiary grade needs to be included (and added to the primary grade) in the Gleason score since a small focus of high-grade carcinoma present in the biopsy may correlate with a significant presence throughout the entire prostate, thus influencing prognosis. Therefore, 3+4+5=8 and not 7, and 2+3+4=6 and not 5. You take the highest and lowest numbers and add them together.
The application of the Gleason score is unreliable in the evaluation of tumors which have been subject to neoadjuvant hormone therapy or radiotherapy. In these cases it is better to refer to the pretreatment Gleason biopsy.
As PCA3 testing has not become a part of routine clinical practice, PSA (glycoprotein produced mainly by the prostate) can currently be considered the only marker used on a routine basis in patients with prostate disease. PSA is however nonspecific, since it can be elevated in the presence not only of malignant lesions, but also of benign ones (e.g. hyperplasia, acute inflammation, infarction, urinary retention), as well as after several diagnostic procedures such as digital rectal examination (DRE), cystoscopy, and prostatic biopsy. In the latter case, increases of up to 50 times may be observed with a slow return to normal values in 30 to 60 days. Therefore, when we want to evaluate therapy-induced changes in PSA, the assay should be done prior to DRE, TRUS, and instrumental procedures in the rectum and colon (e.g. rectoscopy or colonoscopy). In addition, a period of four weeks should pass after prostatic biopsy if the measured serum PSA is to be considered reliable. On the other hand, PSA levels in the bloodstream can decrease following the use of several drugs utilized in the treatment of benign prostatic hyperplasia (BPH). The PSA drops in men who use minoxidil for hair growth. Considering the prevalence of prostate cancer in the population affected by BPH, a drug-induced reduction in PSA can compromise the diagnostic utility of the marker in the presence of malignant tumor. Therefore, to exclude the concomitant presence of the latter, the following is advisable:
PSA is generally evaluated with reference to a threshold value calculated on the basis of the distribution of the marker in normal subjects. The threshold value used is 4 ng/mL, although this value may be considered conventional since it is characterized by low positive and negative predictive values. This is due to several reasons including patient age (PSA tends to increase in the elderly), and the overlap between patients with neoplasm confined to the prostate and patients with BPH who present values ranging from 4 to 10 ng/mL.
The possibility of a positive biopsy for prostate cancer can be correlated with tPSA values. The probability of carcinoma in patients with tPSA of 0.0-4.0 ng/mL is 10%, and in 90% of cases the tumor is confined to the prostate. With a tPSA of 4.0-10.0 ng/mL the probability of carcinoma is 25% with the tumor confined to the prostate in 70% of cases. With a tPSA >10.0 ng/mL the probability of carcinoma is 50%, with the tumor confined to the prostate in 50% of cases.
Adjusting the PSA value on the basis of patient age has been introduced to improve the sensitivity of the marker in young subjects and the specificity in the elderly. The correlation of PSA values by age does not guarantee an acceptable increase in sensitivity and specificity.
Serum PSA exists in various forms, even though most of it is in complex with protease inhibitors such as alpha 1-antichymotrypsin, and only a small amount is present in the free form. The ratio between free PSA (fPSA) and total PSA (tPSA) is defined PSA ratio. The percentage of fPSA is lower in subjects with prostate cancer. Therefore, the percentage of fPSA can be useful in determining which patients should undergo prostatic biopsy. It has been demonstrated that the percentage of fPSA can increase the specificity of tPSA in subjects with a tPSA between 2.5 and 10 ng/mL. The sensitivity and specificity of the percentage of fPSA are independent of the age of the subject undergoing the examination.
PSA velocity measures the changes in PSA over one year, thus making possible a longitudinal evaluation of serum PSA levels. In the first half of the 1990s, the concept was introduced that an increase in tPSA greater than 0.75 ng/mL per year is suggestive of carcinoma.
PSA doubling time measures the rate of change in a different manner, using a logarithmic formula to calculate the time it takes for PSA to double in value. The formula is:
log (2xt) divided by log (final PSA) - log (initial PSA).
PSA doubling time is expressed in months.
PSA density refers to the tPSA divided by the prostate volume expressed in cubic centimeters (cc). The calculation can be made in terms of the total prostate volume (PSA density), or in the terms of the volume of the transition zone, the site of BPH (PSA transition zone density).
Normally, in subjects with a tPSA between 4 and 10 ng/mL a normal PSA density value is 0.15.
Currently it is possible to assay PSA in complex with alpha 1-antichymotrypsin (cPSA).




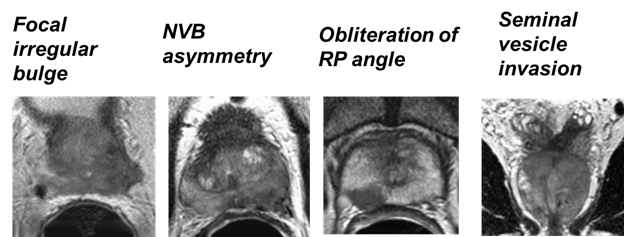
Imaging findings suggesting extraprostatic extension:
![]()

MRI Findings in T3 Disease with Capsular Signs of Involvement
Radiology 1997; 202: 697-702 and 2005; 237: 541-549
Abbreviations: RP = Rectoprostatic angle; NVB = Neurovascular Bundle
T-stage of TNM classification for prostate cancer
|
TX |
Primary tumor cannot be assessed |
|
T0 |
No evidence of primary tumor |
|
T1 |
Clinically inapparent tumor neither palpable nor visible by imaging |
|
T1a |
Tumor incidental histologic finding in 5% or less, or tissue resected |
|
T1b |
Tumor incidental histologic finding in more than 5% of tissue resected |
|
T1c |
Tumor identified by needle biopsy (e.g. because of elevated PSA) |
|
T2 |
Tumor confined within prostate |
|
T2a |
Tumor involves one-half of one lobe or less |
|
T2b |
Tumor involves more than one-half of one lobe but not both lobes |
|
T2c |
Tumor involves both lobes |
|
T3 |
Tumor extends through the prostate capsule |
|
T3a |
Extracapsular extension (unilateral or bilateral) |
|
T3b |
Tumor invades seminal vesicle(s) |
|
T4 |
Tumor is fixed or invades adjacent structures other than seminal vesicles, such as external sphincter, rectum, bladder, levator muscles, and / or pelvis wall |
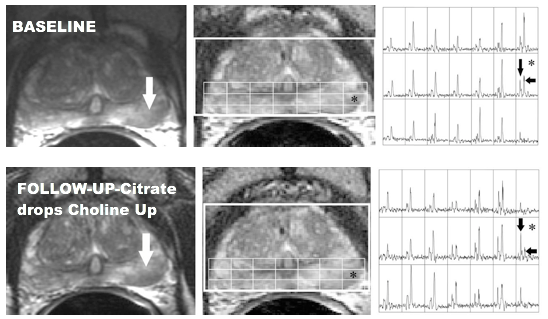
The rationale behind the use of magnetic resonance spectroscopy (MRS) is provided by the demonstration of elevated levels of choline and low levels of citrate in the carcinoma. This is the opposite of normal prostate tissue where the concentration of citrate is high and choline is low. The low concentrations of citrate in the tumor are the result of changes in cellular function and tissue architecture. In fact, the neoplastic cells are less able to synthesize citrate, and the normal glandular epithelium is substituted by the newly formed tissue. High concentrations of choline, which is a component of the cellular membranes, are found in carcinoma of the prostate due to the irregular multiplication of the tumor membranes.
The presence of cancer is hypothesized when the ratio (>0.75) of (Cho+Cr)/Cit in the suspicious zone deviates by more than 2 to 3 standard deviations (SD) with respect to the value obtained in the healthy reference zone. A ratio (>0.86) of (Cho+Cr)/Cit greater than 3 SD with respect to the value of the normal zone is defined as the definite presence of neoplasia. The voxels with a ratio less than 0.75 are defined as normal tissue of the peripheral zone.
A marked reduction to the point of absence of the citrate peak has been observed in cases of high-grade Gleason tumors and a smaller reduction in the peak in low-grade Gleason tumors.
The Key Peaks: Citrate, Creatine, and Choline


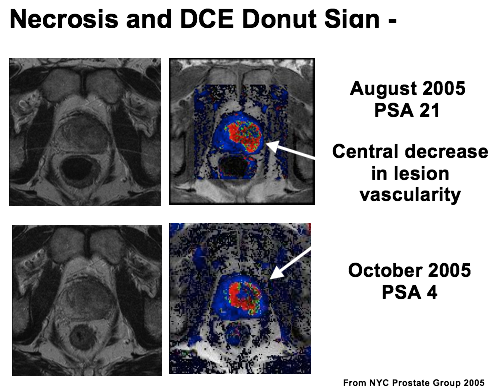
Disease monitoring by MRI/MRSI (e.g. Spectroscopy)
A positive scintigraphy is highly uncommon with PSA levels below 20 ng/mL. The examination is therefore indicated in patients with:
Whole body bone scan - example
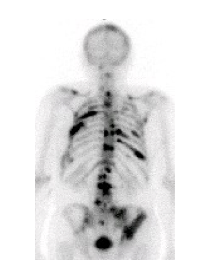
Scintigraphy and Bone Scan Positivity
|
PSA Level |
Positive bone scan |
||
|
< 10 |
0% (0/290) |
0% (0/71) |
0% (0/161) |
|
10-20 |
4.5% (4/88) |
1.6% (1/61) |
2.1% (2/95) |
|
> 20 |
21% (24/112) |
41% (34/82) |
- |
Gleave et al, Urology 1996; 47: 708-12 Rhoden et al, Int Braz J Urol 2003; 29: 121-125 Hirobe et al, Jpn J Clin Oncol 2007
Negative Bone Scintigraphy, Positive CT and MRI

Pearls

CT and Nodal/ Disease Positivity in New Untreated Patients
Huncharek et al, Cancer Invest 1995;13: 31-5 Lee et al. Urology 1999; 54: 490-4
Huncharek et al. Abdom Imaging 1996; 21: 364-7
|
N |
Positive CT |
PSA cut-off |
|
300 |
10 (3%) |
> 20 in 8 |
|
588 |
41 (7%) |
> 15 in 33 |
|
425 |
13 (3%) |
> 30 in 11 |
Comparison of Sonography, MRI and Pathology with Peripepheral Zone Tumor (arrow)

TRUS with Peripheral Zone tumor (arrow)

Choi YJ, Kim JK, Kim N et al (2007) Functional MR imaging of prostate cancer. RadioGraphics 27:63-75
Choyke PL (2006) Prostate cancer imaging: past, present, future. RSNA categorical course in diagnostic radiology. Genitourinary Radiology, pp 35-41
Clase FG, Hricak H, Hattery RR (2004) Pretreatment evaluation of prostate cancer: role of MR imaging and 1H MR spectroscopy. Radiographics 24:S167-180
Fuchsjäger M, Shukla-Dave A, Akin O et al (2008) Prostate cancer imaging. Acta Radiol 49:107-120
Hambrock T, Padhani AP, Tofts PS et al (2006) Dynamic contrast-enhanced MR imaging in the diagnosis and management of prostate cancer. RSNA categorical course in diagnostic radiology. Genitourinary Radiology, pp 61-77
Hricak H, Choyke PL, Eberhardt SC (2007) Imaging prostate cancer: A multidisciplinary perspective. Radiology 243:28-53
Oon SF, Watson RW, O’Leary JJ, and Fitzpatrick JM (2011) Epstein criteria for insignificant prostate cancer. BJU International 108:518-525
Presti JC Jr (2000) Prostate cancer: assessment of risk using digital rectal examination, tumor grade, prostate-specific antigen, and systematic biopsy. Radiol Clin North Am 38:49-58
Shukla-Dave A, Hricak H (2006) MR spectroscopy of prostate cancer: current practices ad techniques. RSNA categorical course in diagnostic radiology. Genitourinary Radiology, pp 53-60
Standring, S (2005) Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 39th Edition. Prostate, pp. 1,301-1,304
Yu KK, Hricak H (2000) Imaging prostate cancer. Radiol Clin North Am 38:59-85
We're on a mission to bring the best online MRI education to the world's radiologists
5400 Kennedy Ave. Cincinnati, OH 45202
M-F 8AM-5PM EST
+1 866-MRI-EDUC (866-674-3382)
education@proscan.com